Leaky Brain Syndrome: Symptoms, Causes, and Solutions
Have you ever heard the term “leaky brain” syndrome? If not, you may be surprised to learn that leaky brain is an increasingly common condition that has been linked to a variety of chronic health issues.
What is Leaky Brain Syndrome?
Leaky brain syndrome is a condition in which the blood brain barrier (BBB) has been damaged, allowing toxins and other harmful substances to enter the brain.
The brain is an amazingly complex machine. It manages every function of your body, including your thoughts, metabolism, digestion, and hormones. Such an important machine needs to be protected from bacteria, toxins, and other foreign invaders. That’s where the blood brain barrier comes in.
The blood brain barrier is a wall between the bloodstream and the brain. It’s composed of a single layer of cells surrounding the brain. These cells are joined together by tight junctions that allow water, oxygen, essential nutrients, and other helpful substances to enter the brain via cerebral blood circulation, while filtering out harmful substances. Thus, the blood brain barrier is said to be “semi-permeable.”
The BBB’s function is very similar to that of the intestinal barrier, the breakdown of which is a key factor in leaky gut syndrome.
Leaky Gut and Leaky Brain Syndrome: a Major Link
You’re probably aware of “leaky gut” syndrome. After all, this term has been around for over a decade. However, it might surprise you to learn that leaky gut and leaky brain are related. That is, both are caused by inflammation, and their mechanisms of development are similar.
Consider this: like the brain, the gut also has a barrier. This intestinal barrier is designed to keep harmful substances from entering the bloodstream. It’s composed of a single layer of epithelial cells connected by inter-epithelial tight junctions that line the length of the gastrointestinal tract.
These tight junctions keep harmful molecules and organisms from escaping into the general bloodstream, while allowing water and nutrients to enter the gastrointestinal system.
By nature, the intestinal barrier is semi-permeable to allow beneficial substances to enter the digestive system. But gut inflammation can increase intestinal permeability, allowing pro-inflammatory substances to enter systemic circulation, causing wide-spread bodily inflammation. This can lead to many chronic health conditions.1
If you have leaky gut syndrome, there’s a good chance you also have leaky brain syndrome. That’s because the systemic inflammation it causes weakens the blood brain barrier. This allows pro-inflammatory cytokines to enter the brain, triggering neurological inflammation.
But research shows that the gut may also exert an independent influence on brain function and inflammation due to the unique properties of the gut brain axis.
Gut Brain Axis and Brain Inflammation
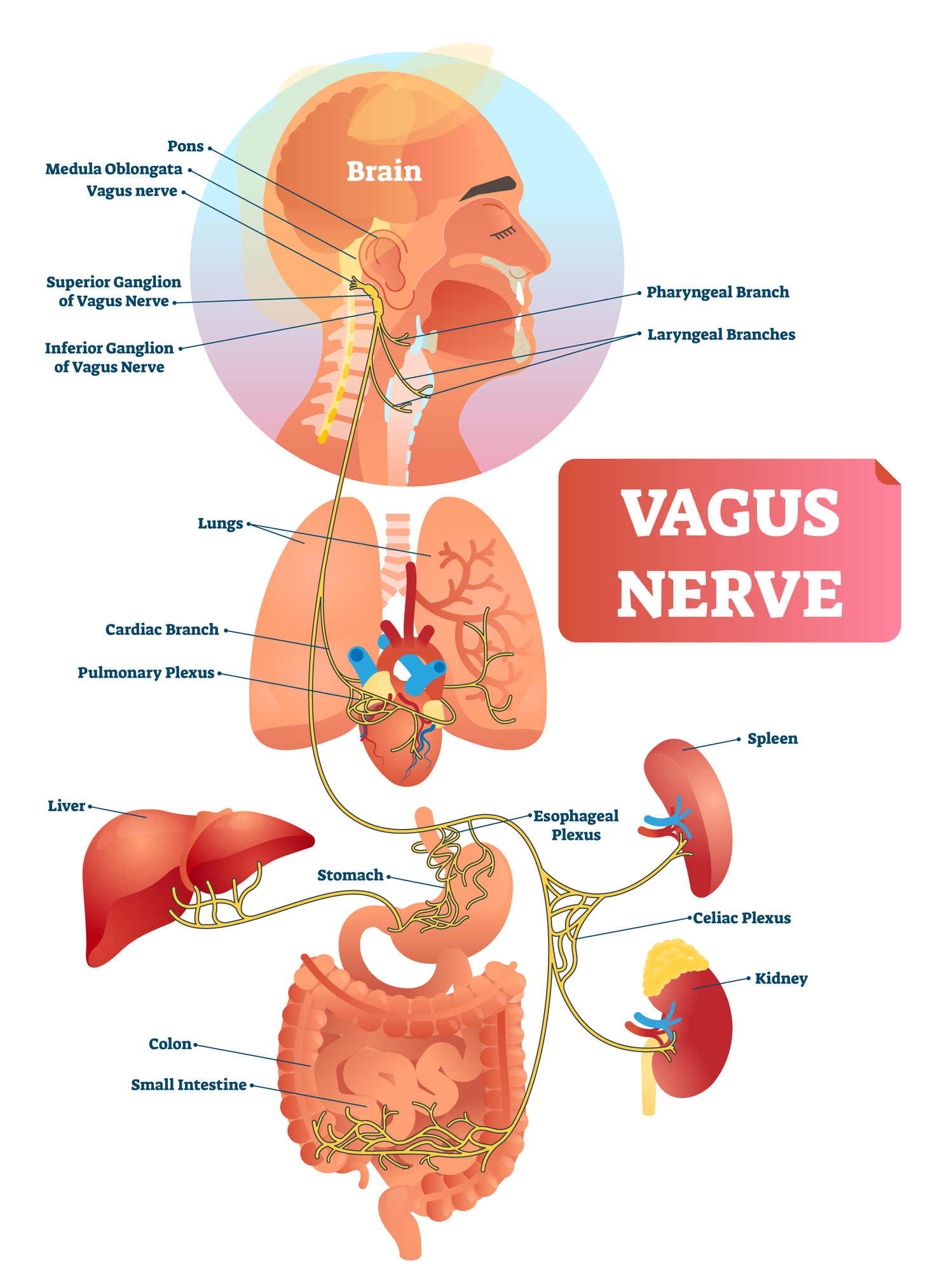
Turns out, the gut and brain continually communicate with each other via the vagus nerve. The vagus nerve is the longest cranial nerve, extending from your brain stem to part of the colon.
Branches of the vagus nerve connect most of the major organs. Through this nerve, the brain receives signals from the rest of the body enabling it to respond to the body’s needs, i.e., release specific hormones, activate the immune response to infections/injuries, etc.
But it also works in reverse: the body receives signals from the brain and reacts accordingly. And this certainly includes the gut. In fact, pre-clinical studies suggest that traumatic brain injury (TBI) can cause “structural and functional” damage to the gastrointestinal tract.2
And growing evidence suggests that the state of your gut can also affect the state of your brain.
In a 2020 study, for instance, researchers noted:
“Changes in gut microbiota can promote enteric and peripheral neurogenic/inflammatory responses, which, in turn, could contribute to neuroinflammation and neurodegeneration in the central nervous system (CNS).”3
Indeed, scientific evidence suggests that gut bacteria modulate inflammatory pathways that in turn may directly influence the state and function of the brain.4
This can lead to brain inflammation.
Dangers of Neurological Inflammation
But why does neurological inflammation matter?
Research suggests that chronic brain inflammation is a key factor in the development of multiple neurological and neurodegenerative disorders. It also plays a role in general health and disease states, as well as mood and emotional dysregulation.
Conditions associated with chronic brain inflammation include:5, 6, 7, 8, 9, 10, 11, 12, 13
Neurological disorders
- Parkinson’s disease
- Alzheimer’s disease
- Huntington’ disease
- Stroke
Mood Disorders
- Depression
- Anxiety
- Bipolar disorder
Mental/Mental Health Disorders
- Autism Spectrum Disorder (ASD)
- Attention Deficit Hyperactivity Disorder (ADHD)
- Borderline Personality Disorder (BPD)
- Post Traumatic Stress Syndrome (PTSD)
Autoimmune Disease
- Arthritis
- Irritable Bowel Disease
- Lupus
- Multiple Sclerosis
Other Health Conditions
- Weight gain/obesity
- Diabetes
- Heart disease
And the list goes on and on.
Early Signs and Symptoms of Leaky Brain Syndrome
The signs/symptoms of leaky brain syndrome are varied and include:
- Brain fog
- Trouble concentrating
- Depression
- Anxiety
- Weight gain/trouble losing weight
- Fatigue
- Memory loss, i.e., failure to remember where you put your keys, etc.
- Mood swings
Long-Term Dangers of Leaky Brain
If leaky brain is not reversed, it can progress into the more serious and debilitating conditions listed in the “Dangers of Neurological Inflammation” section.
What Causes Leaky Brain Syndrome?
Besides leaky gut, there are several other factors that can cause leaky brain syndrome, most of which you can control. Here are just a few of them.
1.Inflammatory Diet
The foods you eat every day are key to the health of your gut, your brain, and the rest of your body.
Regularly eating what has been called the “standard American diet” of overly processed foods, fast foods, and starchy carbs, sugar, and processed fats have been observed in clinical research studies to weaken/damage both the intestinal barrier and the blood brain barrier.
Why?
Well…research suggests that these foods trigger inflammation in our guts, bodies, and ultimately, our brains.
Inflammatory Foods
Foods associated with inflammation include:
Added Sugars
Sugar is a huge player in inflammation.
Multiple preclinical research studies, i.e., animal studies, suggest that a high-sugar diet not only leads to increased gut permeability and inflammation, but it also increases the risk of obesity and insulin resistance.14
Human research trials yielded similar results. For example, one study on human subjects showed that drinking one 375-ml can of soda per day increases inflammatory markers as well as insulin resistance. It also appeared to lead to weight gain in research subjects.15
Refined Starches
Refined starches like white bread, pasta, and rice have been shown to have a similar inflammatory effect on the body as sugar.
For instance, a large population-based cohort study suggests that increased intake of refined sugars and starches increases the risk of dying from an inflammatory disease. This is because they cause oxidative stress that raise inflammatory markers.16
Trans Fats
Trans fats (trans fatty acids) are created by adding hydrogen to liquid vegetable oils, making them more solid. Trans fats are typically listed on food labels as “partially hydrogenated oils.
Manufacturers use trans fats because they’re inexpensive and give foods a preferred taste and texture. It also increases the food’s shelf life. However, trans fats are pro-inflammatory substances that not only increase inflammation, but also increase your risk of heart disease and possibly type 2 diabetes.17
Omega-6 Fatty Acids
Omega-6 fatty acids are essential fats that can only be gotten through your diet. However, some studies suggest that eating too much of them may cause inflammation in the body. Other studies, though, indicate that omega-6 fatty acids have an anti-inflammatory effect on the body, reducing the risk of cardiovascular disease.18
Due to conflicting studies, your best bet is to eat these foods in moderation.
Foods that contain omega-6 fatty acids include vegetable oils and mayonnaise.
Gluten
Gluten is a protein found in wheat and other cereal grains. Unfortunately, it has also been linked to inflammation.
In a review of research published between 1964 and 2016 regarding the health effect of gluten, researchers concluded:
“Gluten affects the microbiome and increases intestinal permeability. It boosts oxidative stress and affects epigenetic behavior. It is also immunogenic, cytotoxic, and proinflammatory.”19
It’s also an often unrecognized food sensitivity, as many people may have gluten sensitivity without realizing it.
Though research is mixed, if you want to reduce or prevent inflammation, eating a gluten free diet is probably a good plan.
2.Environmental Toxins
Toxins are everywhere in our environment. Household cleaners. Air pollution. Pesticides. Processed foods. Plastics. Cosmetics.
Though a necessary part of our industrialized society, environmental toxins build up in our system endangering our health. And studies show that these toxins may lead to leaky brain with resulting brain inflammation.20
3.Chronic Stress
Stress is almost unavoidable in our fast-paced society. But if it turns into chronic stress, it can damage your blood brain barrier.
This is because stress triggers a rush of cortisol. Though useful in the short-term, too much cortisol impairs brain function and degrades an important tight junction protein, compromising the integrity of the BBB. This can lead to leaky brain.21, 22
4.Deficiency of Brain-Boosting Nutrients
According to the Centers for Disease Control, poor nutrition is one of the top causes of preventable chronic diseases.23
And this is particularly true of leaky brain syndrome.
In fact, most people are deficient in these 4 brain-boosting, inflammation-reducing nutrients:
Folate: Also called folic acid, this B vitamin is essential for brain development and brain health. In fact, folate deficiency has been lined to depression and dementia. As King’s College Neurologists stated: “It is becoming clear that folic acid affects mood and cognitive function, especially in older people.”24
Citicoline: A precursor of choline, citicoline is a crucial brain nutrient that increases levels of the neurotransmitter acetylcholine. Citicoline also increases choline levels in the brain. The U.S. Institute of Medicine discovered that: “Choline has a critical role in neurotransmitter function… and studies suggest that choline supplements increase dopamine receptor densities and can alleviate or improve memory impairment.”25
Coenzyme Q10 (CoQ10): Often called a “universal antioxidant,” CoQ10 is an important nutrient for brain health. For example, if the blood brain barrier is breached, CoQ10 may protect the brain from free-radical damage that can trigger neurological inflammation.26
Acetyl-L-Carnitine (ALC): A naturally occurring nutrient, ALC has been shown to have neuroprotective properties. Research shows that it may help reduce neuroinflammation, a key factor in many neurodegenerative diseases.27
Natural Solutions for Leaky Brain
There are several national solutions for leaky brain. Here are just a few of them.
Improve the Quality of Your Diet
Improving the quality of your diet is one of the most important things you can do to prevent or fix leaky brain. Here are a few clinically proven dietary principles that can help defend against inflammation.
Eat Anti-Inflammatory Foods
Eat more of these anti-inflammatory foods: 28
- A variety of vegetables
- Fruits (try to choose low-sugar varieties, e.g., citrus fruits, berries)
- Nuts
- Whole grains
- Foods high in omega-3 fatty acids, e.g., fish, flaxseeds
Be sure to increase your fiber intake, as this has been shown to defend against many health conditions/diseases.
Avoid Inflammatory Foods
Eat fewer inflammatory foods, such as:29
- Heavily processed foods
- Foods with added sugar
- Processed grains, i.e. white bread, white rice
- Saturated fats and trans fatty acids
Reduce Exposure to Environmental Toxins
You cannot totally eliminate toxins from your environment. But you can minimize the toxic load by using natural cleaners and cosmetics, avoiding processed foods, and perhaps moving out of the city to a rural area where there’s less air pollution.
Reduce Stress
Here are a few great ways to relieve stress:
- Meditate for 20 minutes, once or twice a day
- Perform a series of soothing yoga postures (asanas)
- Practice deep breathing and/or progressive muscle exercises
- Go for leisurely walks or bike rides
- Join a group
- Go on a special outing with your friends or significant other
Take SANE Vitaae
This new anti-aging, brain-boosting nutraceutical is the first clinically proven formulation created to heal neurological inflammation. It contains all 4 of the crucial brain-boosting super nutrients — folate, citicoline, acetyl-L-carnitine, and CoQ10 — in the correct combinations and dosages you need to fix leaky brain and brain inflammation.
References
3- Pellegrini C, Antonioli L, Calderone V, Colucci R, Fornai M, Blandizzi C. Microbiota-gut-brain axis in health and disease: Is NLRP3 inflammasome at the crossroads of microbiota-gut-brain communications? Prog Neurobiol. 2020 Aug;191:101806. doi: 10.1016/j.pneurobio.2020.101806. Epub 2020 May 28. PMID: 32473843.
4- Pellegrini C, Antonioli L, Calderone V, Colucci R, Fornai M, Blandizzi C. Microbiota-gut-brain axis in health and disease: Is NLRP3 inflammasome at the crossroads of microbiota-gut-brain communications? Prog Neurobiol. 2020 Aug;191:101806. doi: 10.1016/j.pneurobio.2020.101806. Epub 2020 May 28. PMID: 32473843.
5- Degan D, Ornello R, Tiseo C, Carolei A, Sacco S, Pistoia F. The Role of Inflammation in Neurological Disorders. Curr Pharm Des. 2018;24(14):1485-1501. doi: 10.2174/1381612824666180327170632. PMID: 29589534.
6- Degan D, Ornello R, Tiseo C, Carolei A, Sacco S, Pistoia F. The Role of Inflammation in Neurological Disorders. Curr Pharm Des. 2018;24(14):1485-1501. doi: 10.2174/1381612824666180327170632. PMID: 29589534.
7- Rossi S, Studer V, Motta C, Polidoro S, Perugini J, Macchiarulo G, Giovannetti AM, Pareja-Gutierrez L, Calò A, Colonna I, Furlan R, Martino G, Centonze D. Neurology Sep 2017, 89 (13) 1338-1347; DOI: 10.1212/WNL.0000000000004411
8- Linebeck Institute. Inflammation in mood disorders: a new day or a false dawn? Aug 26, 2019. Accessed May 6, 2021. https://institute.progress.im/en/content/inflammation-mood-disorders-new-day-or-false-dawn
9- Kraybill Odelya. Inflammation and Mental Health Symptoms. Psychology Today. May 31, 2019. Accessed May 6, 2021. https://www.psychologytoday.com/us/blog/expressive-trauma-integration/201905/inflammation-and-mental-health-symptoms
10- Kraybill Odelya. Inflammation and Mental Health Symptoms. Psychology Today. May 31, 2019. Accessed May 6, 2021. https://www.psychologytoday.com/us/blog/expressive-trauma-integration/201905/inflammation-and-mental-health-symptoms
11- Cesar HC, Pellegrini Pisani L. Fatty-acid-mediated hypothalamic inflammation and epigenetic programming, The Journal of Nutritional Biochemistry, Volume 42, 2017, Pages 1-6, ISSN 0955-2863, https://doi.org/10.1016/j.jnutbio.2016.08.008.
12- Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, Zhao X, Sarruf DA, Izgur V, Maravilla KR, Nguyen HT, Fischer JD, Matsen ME, Wisse BE, Morton GJ, Horvath TL, Baskin DG, Tschöp MH, Schwartz MW. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012 Jan;122(1):153-62. doi: 10.1172/JCI59660. Epub 2011 Dec 27. Erratum in: J Clin Invest. 2012 Feb 1;122(2):778. PMID: 22201683; PMCID: PMC3248304.
13- Cai D, Liu T. Hypothalamic inflammation: a double-edged sword to nutritional diseases. Ann N Y Acad Sci. 2011;1243:E1-E39. doi:10.1111/j.1749-6632.2011.06388.
14- Frazier TH, DiBaise JK, McClain CJ. Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. JPEN J Parenter Enteral Nutr. 2011 Sep;35(5 Suppl):14S-20S. doi: 10.1177/0148607111413772. Epub 2011 Aug 1. PMID: 21807932.
15- Aeberli I, Gerber PA, Hochuli M, Kohler S, Haile SR, Gouni-Berthold I, Berthold HK, Spinas GA, Berneis K. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am J Clin Nutr. 2011 Aug;94(2):479-85. doi: 10.3945/ajcn.111.013540. Epub 2011 Jun 15. PMID: 21677052.
16- Buyken AE, Flood V, Empson M, Rochtchina E, Barclay AW, Brand-Miller J, Mitchell P. Carbohydrate nutrition and inflammatory disease mortality in older adults. Am J Clin Nutr. 2010 Sep;92(3):634-43. doi: 10.3945/ajcn.2010.29390. Epub 2010 Jun 23. PMID: 20573797.
17- Mozaffarian D. Trans fatty acids – effects on systemic inflammation and endothelial function. Atheroscler Suppl. 2006 May;7(2):29-32. doi: 10.1016/j.atherosclerosissup.2006.04.007. Epub 2006 May 18. PMID: 16713393.
18- Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ, Engler MM, . Engler MB, Sacks F. Omega-6 Fatty Acids and Risk for Cardiovascular Disease. Circulation. Jan 26, 2009. Vol 119, Issue 6. https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.108.191627
19- Lerner A, Shoenfeld Y, Matthias T. Adverse effects of gluten ingestion and advantages of gluten withdrawal in nonceliac autoimmune disease. Nutr Rev. 2017 Dec 1;75(12):1046-1058. doi: 10.1093/nutrit/nux054. PMID: 29202198.
20- Yegambaram M, Manivannan B, Beach TG, Halden RU. Role of environmental contaminants in the etiology of Alzheimer’s disease: a review. Curr Alzheimer Res. 2015;12(2):116-46. doi: 10.2174/1567205012666150204121719. PMID: 25654508; PMCID: PMC4428475.
21- Van der Kooij MA, Fantin M, Rejmak E, Grosse J, Zanoletti O, Fournier C,Ganguly K,Kalita K, Kaczmarek L, Sandi C. Role for MMP-9 in stress-induced downregulation of nectin-3 in hippocampal CA1 and associated behavioural alterations. Nature Communications, 2014; 5: 4995. Link Here
22- Dudek KA, Dion-Albert L, Lebel M, LeClair K, Labrecque S, Tuck E, Ferrer Perez C, Golden SA, Tamminga C, Turecki G, Mechawar N, Russo SJ, Menard C. Molecular adaptations of the blood-brain barrier promote stress resilience vs. depression. Proc Natl Acad Sci U S A. 2020 Feb 11;117(6):3326-3336. doi: 10.1073/pnas.1914655117. Epub 2020 Jan 23. PMID: 31974313; PMCID: PMC7022213.
23- Centers for Disease Control. Chronic Diseases in America. CDC. Page last reviewed: Jan 12, 2021. Accessed May 7, 2021. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
24- Reynolds EH. Folic acid, ageing, depression, and dementia. BMJ. 2002;324(7352):1512-1515. doi:10.1136/bmj.324.7352.1512
25- Institute of Medicine (US) Committee on Nutrition, Trauma, and the Brain; Erdman J, Oria M, Pillsbury L, editors. Nutrition and Traumatic Brain Injury: Improving Acute and Subacute Health Outcomes in Military Personnel. Washington (DC): National Academies Press (US); 2011. 9, Choline. Available from: https://www.ncbi.nlm.nih.gov/books/NBK209327/
26- Kalayci M, Unal MM, Gul S, Acikgoz S, Kandemir N, Hanci V, Edebali N, Acikgoz B. Effect of coenzyme Q10 on ischemia and neuronal damage in an experimental traumatic brain-injury model in rats. BMC Neurosci. 2011 Jul 29;12:75. doi: 10.1186/1471-2202-12-75. PMID: 21801363; PMCID: PMC3160960.
27- Traina G. The neurobiology of acetyl-L-carnitine. Front Biosci (Landmark Ed). 2016 Jun 1;21:1314-29. doi: 10.2741/4459. PMID: 27100509.
28- Giugliano D, Ceriello A, Esposito K. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome, Journal of the American College of Cardiology, Volume 48, Issue 4, 2006, Pages 677-685, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2006.03.052.
29- Giugliano D, Ceriello A, Esposito K. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome, Journal of the American College of Cardiology, Volume 48, Issue 4, 2006, Pages 677-685, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2006.03.052.