Diabesity: Understanding the Global Epidemic Transforming Modern Health
Diabetes and obesity are two of the most pressing health challenges of our time. When they occur together, the condition is known as diabesity. This term describes more than the overlap of two chronic diseases; it reflects a deeper metabolic crisis that links excess body weight with insulin resistance, impaired glucose tolerance, and the development of type 2 diabetes. Individuals with obesity and insulin resistance are at increased risk to develop diabetes, as metabolic dysfunction can progress to overt disease if not addressed. As the rates of obesity continue to climb worldwide, so too does the burden of diabetes, cardiovascular disease, and other obesity related diseases that compromise human health.
At SANEMD, we believe that understanding diabesity is the first step toward reclaiming metabolic health. This article provides a comprehensive perspective on the origins, risks, and strategies for prevention and management of diabesity, using the latest insights from clinical nutrition, metabolic science, and public health.
What Does Diabesity Mean?
The word diabesity was first coined by Dr. Ethan Sims in the mid-1970s to describe the close and inescapable link between obesity and diabetes. While once considered separate conditions, medical evidence now demonstrates that obesity and insulin resistance share common molecular mechanisms, making it difficult to address one without considering the other.
In clinical terms, diabesity encompasses individuals who have obesity (measured through body mass index and waist circumference) alongside metabolic dysfunction, including impaired glucose tolerance, hepatic insulin resistance, and elevated serum levels of free fatty acids. The obese phenotype in diabesity is characterized by distinct metabolic and cardiovascular features that influence disease progression and clinical outcomes, setting it apart from other metabolic conditions. Together, these metabolic abnormalities increase risk factors for type 2 diabetes, cardiovascular disease, and heart failure.
Why Obesity and Diabetes Are Interconnected
The connection between obesity and diabetes is rooted in how excess adiposity affects the body’s ability to regulate glucose. Obese individuals often accumulate visceral adiposity, the metabolically active fat that surrounds internal organs. This type of fat releases fatty acids and inflammatory cytokines that impair insulin action, reduce insulin secretion, and disrupt glucose homeostasis.
When obesity persists, the result is insulin resistance. The body compensates by producing more insulin, but over time, this mechanism fails. Insulin secretion cannot keep pace with demand, leading to impaired glucose tolerance and eventually type 2 diabetes mellitus. This cycle is why diabesity is often referred to as a global epidemic—a modern convergence of lifestyle, genetics, and environment.
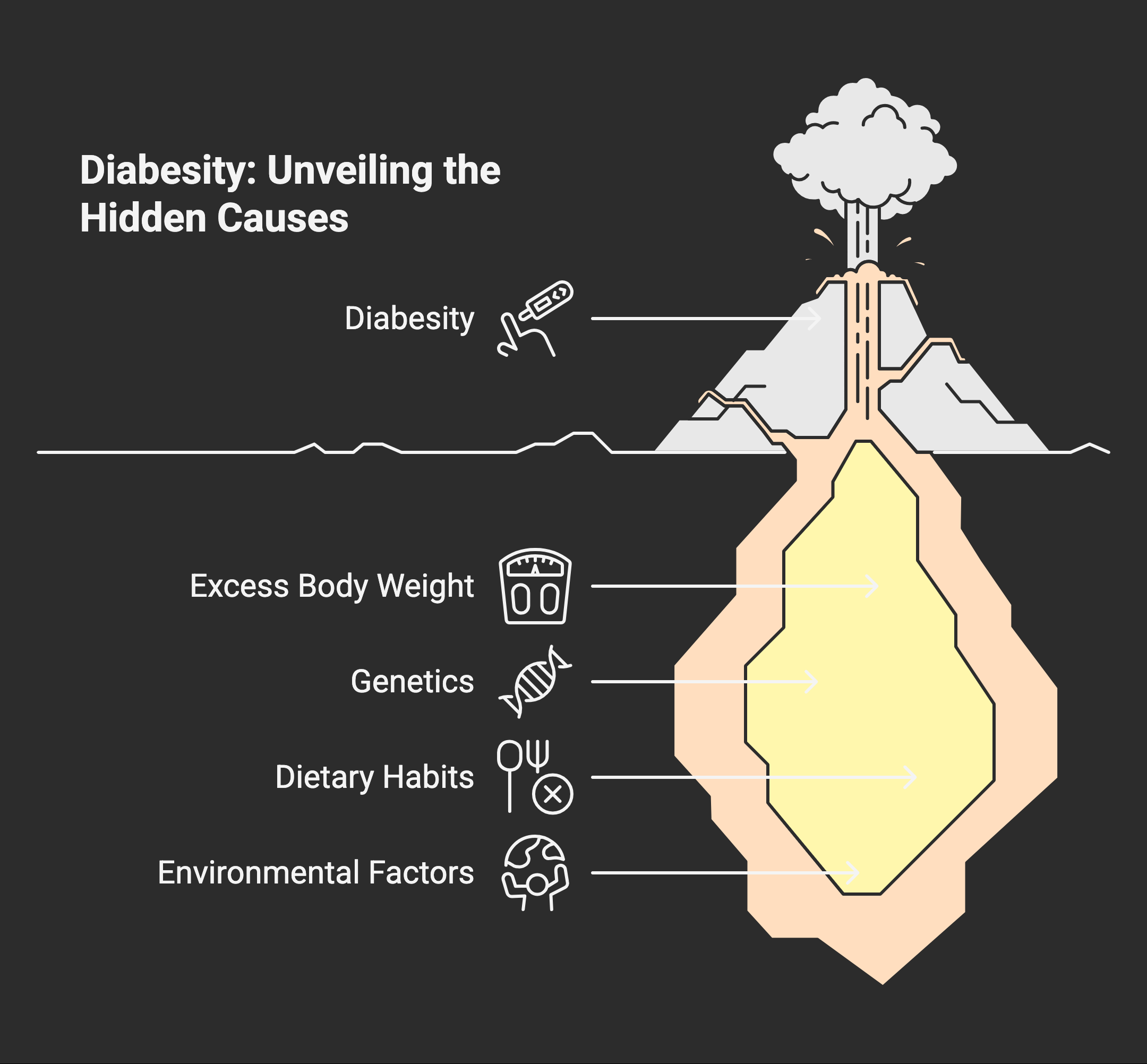
Causes of Diabesity
The causes of diabesity are multifactorial, involving both biology and behavior:
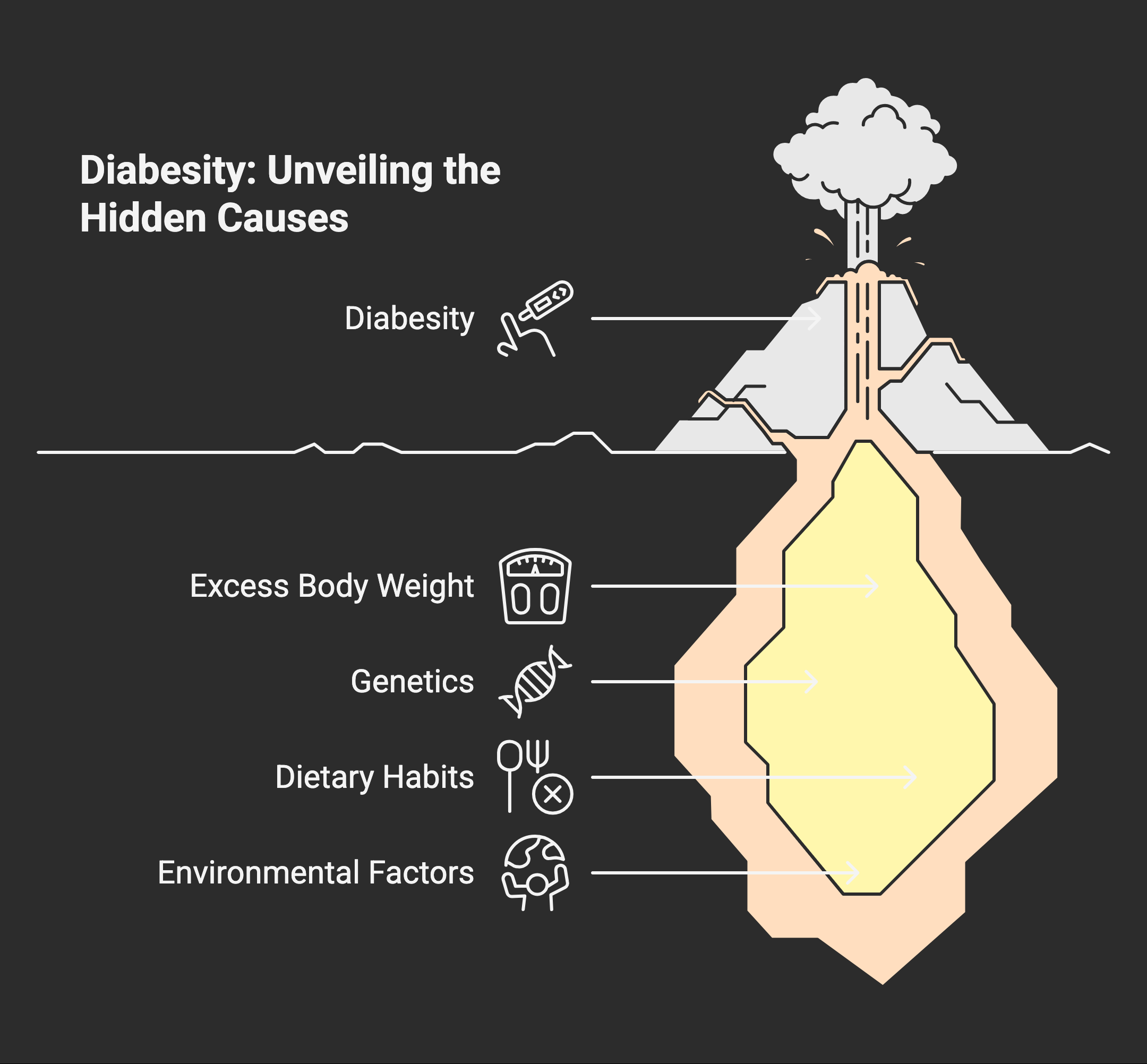
1. Excess Body Weight and Energy Balance
Chronic positive energy balance—where calories consumed exceed calories expended—leads to weight gain, increased adiposity, and eventually severe obesity. Physical inactivity worsens this imbalance, and the sympathetic nervous system often adapts in ways that encourage fat storage.
2. Genetics and Family History
A family history of diabetes or obesity raises the likelihood of developing diabesity. Genetic predisposition influences appetite regulation, fat distribution, and insulin action, though lifestyle factors remain equally important.
3. Diet and Clinical Nutrition
High intake of processed foods, refined sugars, and unhealthy fats disrupts metabolic health. Clinical nutrition studies confirm that excess fatty acids, especially when circulating as free fatty acids, impair insulin sensitivity and contribute to chronic exposure that drives metabolic syndrome.
4. Environmental and Socioeconomic Factors
Urban living, limited access to healthy food, and reduced physical activity all heighten risk factors for diabesity. Stress and central nervous system overstimulation may also affect appetite regulation and contribute to weight gain.
Difference Between Diabetes and Diabesity
While diabetes refers specifically to disorders of blood glucose regulation, diabesity captures the broader picture: the presence of obesity and diabetes together, driven by insulin resistance and metabolic dysfunction.
- Diabetes may develop in individuals with a normal BMI, though type 2 diabetes is far more common among obese adults.
- Diabesity highlights the overlap, emphasizing how increased adiposity and metabolic syndrome accelerate the risk of type 2 diabetes and related cardiovascular events.
This distinction matters clinically because diabetic patients with obesity face greater complications, including coronary artery disease, ischaemic heart disease, and heart failure. Obese patients also show increased risk of impaired cardiac function, cardiac steatosis, and reduced ejection fraction, measurable through cardiac magnetic resonance or computed tomography scans.
The Scope of the Global Epidemic
The rise of diabesity is staggering. Worldwide, rates of obesity have more than tripled since the 1970s, and type 2 diabetes cases have increased in parallel. Public health experts now describe diabesity as a global epidemic, one that threatens to overwhelm healthcare systems with obesity related diseases, metabolic syndrome, and cardiovascular disease.
The epidemic is fueled by:
- Increased consumption of energy-dense foods
- Physical inactivity and sedentary jobs
- Longer lifespans combined with poor lifestyle habits
- Genetic susceptibility amplified by environmental triggers
For obese individuals, these trends translate into higher risk factors for diabetes, heart disease, and long-term complications affecting the central nervous system, endothelial function, and even incretin hormones that regulate appetite and insulin action.
Risk Factors That Drive Diabesity
Understanding risk factors allows for targeted prevention:
- Body Mass Index (BMI): A BMI over 30 significantly raises the chance of insulin resistance and developing diabetes.
- Waist Circumference: Central obesity is a stronger predictor of cardiovascular disease and type 2 diabetes than overall body weight.
- Family History: Genetic predisposition combined with lifestyle risks magnifies vulnerability.
- Physical Activity Levels: Physical inactivity reduces insulin action and impairs glucose homeostasis.
- Dietary Patterns: High sugar and fat intake increase free fatty acids and impair clinical nutrition outcomes.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS face higher risks due to hormonal imbalance and metabolic dysfunction.
These risk factors explain why obese adults and obese patients require earlier intervention, preventive services task force screenings, and consistent monitoring of blood pressure, serum levels, and glycemic control.
Health Consequences of Diabesity
The convergence of obesity and type 2 diabetes—known as diabesity—brings with it a host of serious health consequences that extend far beyond elevated blood sugar. For obese patients, the combination of increased body weight and insulin resistance dramatically raises the risk of developing metabolic syndrome, a cluster of conditions that includes high blood pressure, abnormal lipid levels, and impaired glucose tolerance. These factors collectively set the stage for cardiovascular disease, coronary artery disease, and heart failure, making diabesity a leading contributor to global morbidity and mortality.
One of the key drivers of these complications is the chronic elevation of free fatty acids in the bloodstream. High levels of free fatty acids not only worsen insulin resistance but also contribute to hepatic insulin resistance, further disrupting glucose homeostasis and increasing the likelihood of developing type 2 diabetes mellitus. Visceral adiposity—excess fat stored around the abdominal organs—plays a particularly harmful role, as it is closely linked to both metabolic syndrome and the progression of cardiovascular disease.
Body mass index (BMI) remains a critical measure for assessing overall body weight and identifying individuals at increased risk. A high BMI, especially when accompanied by a large waist circumference or elevated total body fat, signals a greater likelihood of obesity-related diseases, including ischaemic heart disease, polycystic ovary syndrome, and cardiac steatosis. These conditions can lead to reduced cardiac function, impaired endothelial function, and a higher incidence of cardiovascular events.
For those with severe obesity, bariatric surgery offers a powerful tool for weight reduction and improved diabetes management. However, it is not a standalone solution; sustained weight loss and healthy weight maintenance require ongoing commitment to clinical nutrition, physical activity, and regular medical follow-up. Combination therapy—including medications that target incretin hormones and appetite regulation—can further enhance metabolic benefits and support long-term health.
Early intervention is essential. The preventive services task force recommends routine screening for diabetes and obesity, especially in individuals with a family history or genetic predisposition. Monitoring serum levels of key biomarkers, such as incretin hormones, and utilizing advanced imaging techniques like magnetic resonance imaging and computed tomography, can help track disease progression and guide treatment adjustments.
The global epidemic of diabesity demands a coordinated response. Public health campaigns, education, and research are vital to raising awareness and promoting healthy weight management across populations. Addressing energy balance, appetite regulation, and the roles of the central and sympathetic nervous systems in weight gain are all crucial for effective prevention and treatment.
Ultimately, the health consequences of diabesity underscore the need for a comprehensive, multifaceted approach. By prioritizing weight loss, regular physical activity, and evidence-based clinical nutrition, individuals can reduce their risk of serious complications and improve both cardiac function and overall human health. For diabetic patients and obese individuals alike, early intervention and sustained lifestyle changes are the keys to breaking the cycle of diabesity and achieving lasting metabolic health.
How Diabesity Impacts the Heart
The link between diabesity and heart disease is clear. Excess weight, particularly visceral adiposity, contributes to coronary artery disease, ischaemic heart disease, and heart failure. Cardiac MR and cardiac magnetic resonance imaging show evidence of cardiac steatosis—fatty infiltration of the heart—that reduces ejection fraction and impairs cardiac function.
Diabetic patients with severe obesity are more likely to suffer cardiovascular events. For obese subjects, this risk is compounded by elevated blood pressure, abnormal serum levels of triglycerides, and impaired endothelial function. Sustained weight loss has been shown to restore some cardiac function and reduce risk of future cardiovascular disease.
Treatment and Management Strategies
Weight Loss and Weight Reduction
Sustained weight loss remains the cornerstone of diabesity management. Clinical trials demonstrate that even modest weight reduction improves insulin sensitivity, restores glucose homeostasis, and reduces cardiovascular risk factors. Approaches to help patients lose weight include:
- Balanced diets targeting total body fat reduction
- Increased physical activity to restore energy balance
- Combination therapy of nutrition counseling, behavioral support, and in some cases medication
Bariatric Surgery
For obese patients with severe obesity and type 2 diabetes, bariatric surgery has shown remarkable metabolic benefits. Procedures reduce body weight, improve insulin secretion, and often lead to diabetes remission. Long-term studies confirm bariatric surgery lowers cardiovascular events and supports sustained weight loss, though it requires careful follow-up and clinical nutrition planning.
Pharmacological Interventions
Medications targeting appetite regulation, incretin hormones, and insulin action are expanding options for diabesity management. These treatments support weight reduction and glycemic control, but must be integrated with lifestyle changes for full beneficial effects.
Pro Tip: Prevention Is the Best Treatment
While therapies exist, prevention of diabesity offers the greatest potential impact. Addressing risk factors early—through healthy weight maintenance, physical activity, and balanced clinical nutrition—delivers metabolic benefits that reduce the likelihood of obesity and diabetes progressing into diabesity.
The Role of SANEMD
In the middle of this global epidemic, SANEMD provides clarity on how obesity and diabetes intersect to form the condition we know as diabesity. By focusing on evidence-based strategies for weight loss, diabetes management, and prevention of obesity related diseases, SANEMD equips patients and practitioners with practical tools to combat one of the greatest threats to modern human health.
The Future of Diabesity Care
Looking forward, innovation in computed tomography imaging, molecular mechanisms research, and pharmacology will expand our ability to understand diabesity. From improved cardiac function monitoring to deeper insight into how the central nervous system regulates appetite, science continues to uncover opportunities for earlier intervention and better outcomes.
Yet despite advances, lifestyle remains at the heart of the solution. Physical activity, weight reduction, healthy nutrition, and preventive services must remain the focus for populations at increased risk. Every small step toward weight loss or improved insulin sensitivity creates beneficial effects for long-term health.
Final Word
Diabesity is more than a medical term; it is a reflection of the intertwined epidemics of obesity and diabetes. By addressing insulin resistance, supporting weight loss, and reducing risk factors for cardiovascular disease, individuals can reclaim their health and break free from the cycle of metabolic dysfunction.
SANEMD remains committed to providing balanced, medically accurate perspectives on this global epidemic, reminding us that while the challenge is vast, the solutions are within reach. With consistent attention to clinical nutrition, physical activity, and sustained weight loss, diabesity can be prevented, managed, and overcome.