Irritable Bowel Syndrome: IBS Mucus, Symptoms, Causes, and Treatment
Have you ever found yourself grappling with those nagging abdominal discomforts, bloating, and unpredictable shifts in your bowel routine? It’s like an unwelcome guest crashing your daily life, leaving you perplexed and frustrated.
Welcome to the perplexing realm of irritable bowel syndrome (IBS), a persistent hitch in the functioning of your large intestine. IBS is one of the most common bowel disorders. Among its many quirks, mucus production stands out as a notable player, a silent orchestrator in the realm of gut health.
Understanding the intricate dance between IBS and mucus production is pivotal. It unveils the mysteries behind those symptoms, shedding light on a condition often veiled in confusion and uncertainty. So, let’s embark on this journey together, decoding the subtle cues and exploring effective strategies to navigate the labyrinth of IBS management.
Overview: Irritable Bowel Syndrome and Mucus Production
Diving into the intricate dynamics of irritable bowel syndrome (IBS) reveals a complex interplay between the gut and the brain, stirring up a whirlwind of digestive discord.
Picture this: a functional GI disorder that throws the gut-brain axis off balance, triggering a symphony of sensitivity and erratic muscle contractions along the digestive tract. The result? A medley of symptoms like abdominal pain, bloating, and the unpredictable dance between diarrhea and constipation.
The enigmatic origins of IBS continue to puzzle experts, yet whispers suggest that certain individuals harbor a hypersensitive digestive system primed to react to stressors or dietary triggers.
The role of mucus in the GI Tract
Enter mucus, the unsung hero of the gastrointestinal (GI) realm. This clear, viscous liquid isn’t just another bodily secretion—it’s a guardian angel, cocooning delicate GI tissues from harm’s way. Not only does mucus act as a shield against nasties lurking in your gut, but it also greases the wheels, facilitating the smooth journey of food through the digestive maze.
But in the tumultuous world of IBS, mucus takes on a new role—one that’s both protagonist and antagonist. The delicate balance of mucus production can tilt, leading to a surge or decline in its levels. Cue the onset of abdominal woes—pain, bloating, and those pesky shifts in bowel habits.
To pinpoint IBS with its mucus-related nuances, medical sleuths must don their detective hats, sifting through patient histories, conducting meticulous physical exams, and ruling out imposters using the Rome IV criteria.
How IBS affects mucus production
Now, how does IBS wield its influence over mucus production? The answer lies in the intricate tango between the brain and the gut. When communication falters, the gut muscles may go into overdrive, triggering spasms and cramps in the lower abdomen. And what follows? A surge in mucus production amplifies the chorus of abdominal discomfort, bloating, and the erratic rhythm of bowel movements.
The telltale sign? The appearance of mucus in stool is a hallmark of IBS. This uptick in mucus production doesn’t just fuel the fire; it fans the flames, intensifying existing symptoms and muddying the waters of diagnosis and management.
So, dear reader, unraveling the nexus between IBS and mucus production isn’t just a quest for knowledge—it’s a lifeline for those grappling with the relentless grip of this debilitating disorder.
Common IBS Symptoms Related to Mucus
For those navigating the labyrinth of irritable bowel syndrome (IBS), the journey is fraught with a myriad of symptoms, all intricately linked to mucus production. Recognizing these telltale signs is paramount, paving the path to accurate diagnosis and tailored management strategies—a beacon of hope for those seeking relief and reclaiming their quality of life.
Let’s unravel the tapestry of symptoms commonly associated with IBS and mucus production.
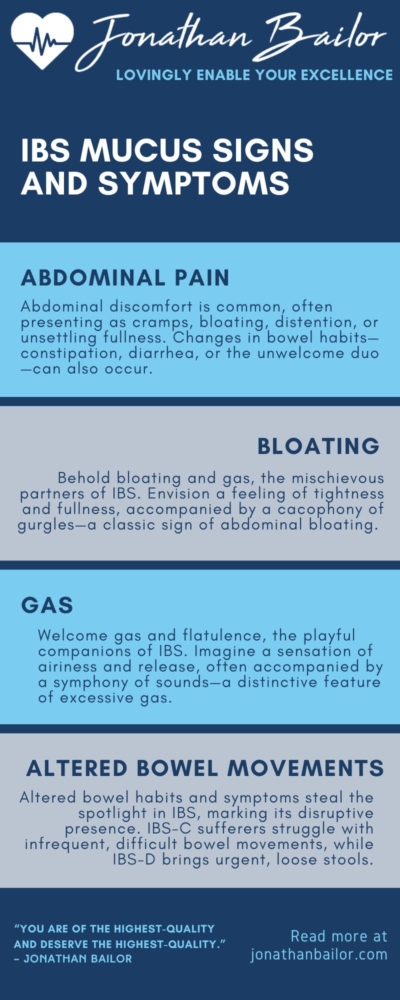
Abdominal Pain and Discomfort
Abdominal pain and discomfort take center stage in this intricate dance, often presenting as cramps, bloating, distention, or unsettling fullness. And the plot thickens with changes in bowel habits—constipation, diarrhea, or the unwelcome duo—leaving individuals grappling with the unpredictable rhythms of their gut.
The culprit? Extra-sensitive nerves in the gut, orchestrating a symphony of discomfort that ebbs and flows with the tides of digestion. But the plot twist lies in the complex relationship between abdominal pain and bowel movements—sometimes relieved, sometimes exacerbated—a puzzle begging to be solved.
Bloating and Gas
Enter bloating and gas, the mischievous sidekicks of IBS. Picture a sensation of tightness and fullness, accompanied by a symphony of wind—a hallmark of abdominal bloating. And let’s not forget flatulence, the inevitable consequence of an uncoordinated dance of bowel contractions and fermenting food trapped within pockets of gut imbalance.
Altered Bowel Habits
But it’s the altered bowel habits and bowel symptoms that truly steal the spotlight—a hallmark of IBS’s disruptive presence. For those with IBS-C, having a bowel movement is difficult and infrequent, while IBS-D brings forth a torrent of urgency and loose stools.
There are other symptoms, too, but the ones above are the most common. Understanding these nuances is the key to unlocking the mysteries of IBS, empowering individuals to navigate their condition with grace and resilience. So, dear reader, arm yourself with knowledge, for it is the greatest weapon in the battle against the enigmatic forces of irritable bowel syndrome.
Diagnosing IBS with Mucus-Related Symptoms
Unlocking the intricate connection between irritable bowel syndrome (IBS) and its telltale altered bowel habits is paramount for steering individuals toward effective diagnosis and management. By identifying and sidestepping potential triggers—be it specific foods or stressors—those grappling with IBS can reclaim control over their digestive woes and forge a path toward a better quality of life.
But to diagnose IBS, especially when mucus-related symptoms come into play, doctors run into many brick walls. The symptoms often mimic those of other conditions, like celiac disease and lactose intolerance, cloaking the true culprit and complicating the diagnostic journey. To unravel this tangled web, healthcare professionals must embark on a thorough investigation, armed with the Rome IV criteria as their compass.
Let’s break down the diagnostic process step by step, shedding light on the meticulous approach required to uncover the mysteries of IBS with mucus-related symptoms.
Medical History and Physical Exam
Medical history and physical examination take center stage in this detective saga. From probing into family medical backgrounds to scrutinizing dietary patterns and mealtime dramas, no stone is left unturned. A careful physical examination serves as the eyes and ears, seeking clues that may hint at alternative diagnoses lurking beneath the surface.
Ruling Out Other Conditions
But the quest doesn’t end there—ruling out imposters is paramount. Inflammatory bowel disease (IBD), colorectal cancer, and a host of non-GI conditions loom on the horizon, their symptoms masquerading as IBS’s signature woes. Blood tests, stool samples, and X-rays serve as investigative tools, banishing these pretenders from the diagnostic spotlight.
Rome IV Criteria
Enter the Rome IV criteria—a beacon of clarity amidst the diagnostic haze. Recurrent abdominal pain, a faithful companion for at least one day per week over the past three months, must be coupled with two or more telltale signs: defecation-related woes, shifts in stool frequency, or alterations in stool appearance.
With these criteria as their guiding stars, healthcare professionals can confidently navigate the murky waters of IBS diagnosis, paving the way for tailored treatment and management strategies. And thus, armed with knowledge and clarity, individuals with IBS can embark on a journey toward reclaiming their well-being and embracing a brighter tomorrow.
Managing IBS and Mucus Production
Navigating the maze of irritable bowel syndrome (IBS) and its intricate dance with mucus production demands a multifaceted approach—one tailored to the unique needs and symptoms of each individual. Once the diagnosis is firmly in place, a plethora of strategies await, poised to alleviate symptoms and pave the path toward a brighter, symptom-free tomorrow.
Let’s embark on this journey of empowerment, exploring the myriad avenues of IBS management, from dietary tweaks to lifestyle overhauls and beyond.
Dietary Modifications
Dietary modifications emerge as stalwart allies in the battle against IBS symptoms. Whether bidding adieu to gluten, a common food intolerance, embracing the low FODMAP lifestyle, or stocking up on fiber-rich foods, the right dietary regimen can relieve symptoms and work wonders in taming abdominal distress, bloating, and bowel irregularities. Conversely, eating gluten and other trigger foods can make symptoms worse.
Lifestyle Changes
But the quest for relief doesn’t end there—lifestyle changes beckon, offering a holistic approach to IBS management. From the serene shores of regular exercise to the tranquil realms of stress management, there are a myriad of paths to explore. Yoga, meditation, and deep breathing exercises hold promise for soothing frazzled nerves, while consistent sleep, meal, and exercise routines lay the groundwork for lasting symptom relief.
Medications and Therapies
Yet, for some, the journey may require additional reinforcements—enter medications and therapies. From antidiarrheals to smooth muscle relaxants, a pharmacopeia of options awaits, each tailored to target specific symptoms and restore balance to the digestive symphony.
But here’s the clincher—there’s no one-size-fits-all solution. Open communication between patients and healthcare professionals is key, guiding the development of a management plan finely tuned to the individual’s needs.
So, dear reader, as you navigate the labyrinth of IBS and mucus production, remember this: you’re not alone. With the proper support, guidance, and a dash of perseverance, relief is within reach. Embrace the journey, empower yourself with knowledge, and reclaim control over your well-being. A brighter, symptom-free tomorrow awaits.
Potential Complications and Risks
Navigating the terrain of irritable bowel syndrome (IBS) isn’t just about managing physical symptoms—it’s also about bracing oneself for potential complications and risks that may lurk beneath the surface. While IBS is often considered a mild condition, its impact on quality of life can be profound, calling attention to a host of potential complications and risks that demand vigilant awareness.
Let’s delve into the shadows, shedding light on the potential pitfalls that individuals with IBS may encounter along their journey.
Hemorrhoids and Fissures
Hemorrhoids and anal fissures emerge as common adversaries, particularly for those grappling with constipation-predominant IBS. These pesky companions—swollen veins and tiny tears—can wreak havoc, causing pain, discomfort, and even bleeding.
The culprit? Straining during bowel movements, a frequent accomplice in the realm of IBS-related woes.
Infections and Inflammation
But the plot thickens with infections and inflammation, potential triggers for post-infectious IBS. Bacterial, viral, or parasitic invaders can incite a cascade of immune responses, setting the stage for chronic inflammation in the digestive tract.
And the fallout? Exacerbated IBS symptoms and a heightened risk of complications, including the dreaded hemorrhoids and anal fissures.
Mental Health Effects
Yet, the impact of IBS extends beyond the confines of the physical realm, casting a shadow over mental health. Anxiety, depression, and a myriad of psychiatric comorbidities often accompany the tumult of IBS, casting a pall over one’s well-being.
The symbiotic relationship between mental health and IBS symptoms only serves to deepen the complexity of the condition, underscoring the importance of a holistic approach to management.
But fear not, dear reader, for knowledge is power. By arming yourself with awareness of these potential complications and risks, individuals with IBS can forge a path toward proactive management.
Through open dialogue with healthcare professionals and mental health specialists alike, a comprehensive management plan can be crafted—one that addresses both the physical and emotional dimensions of IBS.
So, as you traverse the terrain of IBS, remember this: you’re not alone. You can navigate the shadows and emerge stronger on the other side with vigilance, awareness, and a steadfast commitment to holistic well-being.
FAQ: Understanding Irritable Bowel Syndrome (IBS)
Q1: What is irritable bowel syndrome (IBS), and what are its common symptoms?
A1: Irritable bowel syndrome (IBS) is a chronic gastrointestinal disorder characterized by a cluster of symptoms that affect the large intestine. Common symptoms of IBS include abdominal pain or discomfort, bloating, and alterations in bowel habits such as diarrhea, constipation, or a combination of both.
Individuals with IBS may also experience urgency or a feeling of incomplete evacuation after bowel movements. It’s important to note that symptoms can vary in severity and may fluctuate over time.
Q2: What causes irritable bowel syndrome (IBS), and who is at risk?
A2: The exact cause of IBS is not fully understood, but it’s believed to involve a combination of factors, including abnormalities in gut motility, sensitivity to certain foods, changes in gut bacteria, and a heightened response to stress or psychological factors.
While anyone can develop IBS, certain risk factors may increase susceptibility, such as a family history of IBS, female gender, younger age, and mental health conditions like anxiety or depression.
Q3: How is irritable bowel syndrome (IBS) diagnosed?
A3: Diagnosing IBS typically involves a thorough medical history review, physical examination, and the exclusion of other gastrointestinal conditions with similar symptoms. Healthcare professionals may utilize diagnostic criteria such as the Rome IV criteria, which specify the presence of recurrent abdominal pain or discomfort for at least one day per week over the past three months, along with other characteristic symptoms.
Additional tests, such as blood tests, stool samples, and imaging studies, may be performed to rule out other conditions and confirm an IBS diagnosis.
Q4: What are the treatment options for irritable bowel syndrome (IBS)?
A4: Treatment for IBS aims to alleviate symptoms and improve quality of life. Dietary modifications like following a low FODMAP diet or avoiding trigger foods may help manage symptoms like bloating and abdominal discomfort. Lifestyle changes, including stress management techniques and regular exercise, can also play a crucial role in symptom control.
In some cases, medications such as antispasmodics, laxatives, or antidepressants may be prescribed to target specific symptoms or underlying mechanisms contributing to IBS.
Q5: Are there any potential complications or risks associated with irritable bowel syndrome (IBS)?
A5: While IBS is generally considered a benign condition, it can impact quality of life and may lead to potential complications. Common complications of IBS include hemorrhoids, anal fissures, and changes in mental health, such as anxiety or depression. Additionally, individuals with IBS may be at increased risk of developing other gastrointestinal conditions like inflammatory bowel disease (IBD) or colorectal cancer.
Individuals with IBS must know these potential risks and work closely with healthcare professionals to manage their condition effectively.
Summary
In summary, understanding the intricate link between irritable bowel syndrome (IBS) and mucus production is paramount for navigating the complexities of this condition. By recognizing the telltale symptoms and potential risks associated with IBS, individuals can empower themselves to take charge of their health and well-being.
From obtaining an accurate diagnosis to implementing tailored management strategies, collaboration with healthcare professionals is key. By adopting a proactive approach and addressing potential complications head-on, individuals with IBS can pave the way toward a better quality of life.
In the end, knowledge serves as the cornerstone of effective management. Armed with awareness and a commitment to proactive care, those living with IBS can reclaim control and embark on a journey toward a brighter, healthier tomorrow.