Acid Reflux and GERD: Causes and Solutions
Acid reflux occurs when stomach acid or bile flows back up the esophagus. This happens when the lower esophageal sphincter (LES), a muscular ring at the low end of the esophagus, relaxes abnormally.
The lower esophageal sphincter connects the esophagus to the stomach. It remains closed most of the time, opening only to let food pass into the stomach or to release stomach gas.
If the lower esophageal sphincter is weakened, it cannot close properly. This allows stomach acid to reflux back up the esophagus.
This causes a burning sensation in the chest area along with other unpleasant symptoms.
Everyone experiences acid reflux from time to time. It can occur after eating a large meal, which stretches the stomach and puts pressure on the LES. This causes it to temporarily loosen and allow stomach contents to flow back up into the food pipe.
Acid reflux is quite common, regularly affecting 20% of those living in Western countries.1
Though physically unpleasant, occasional reflux usually doesn’t lead to other health problems. Frequent acid reflux, however, can be a sign of gastroesophageal reflux disease (GERD) that can eventually cause serious health problems if untreated.
What is Gastroesophageal Reflux Disease (GERD)
GERD is a serious form of acid reflux. It is a chronic condition characterized by frequent acid reflux, occurring at least twice a week. The symptoms can be mild, moderate, or severe. Regardless of severity of symptoms, however, GERD irritates and can eventually inflame the lining of the esophagus.
The number of people who suffer from GERD is hard to determine. This is because many people who experience symptoms of GERD don’t seek medical attention. A 2014 system review estimates the prevalence of GERD is 15%-30% in the U.S. 2, though this is likely a conservative estimate.
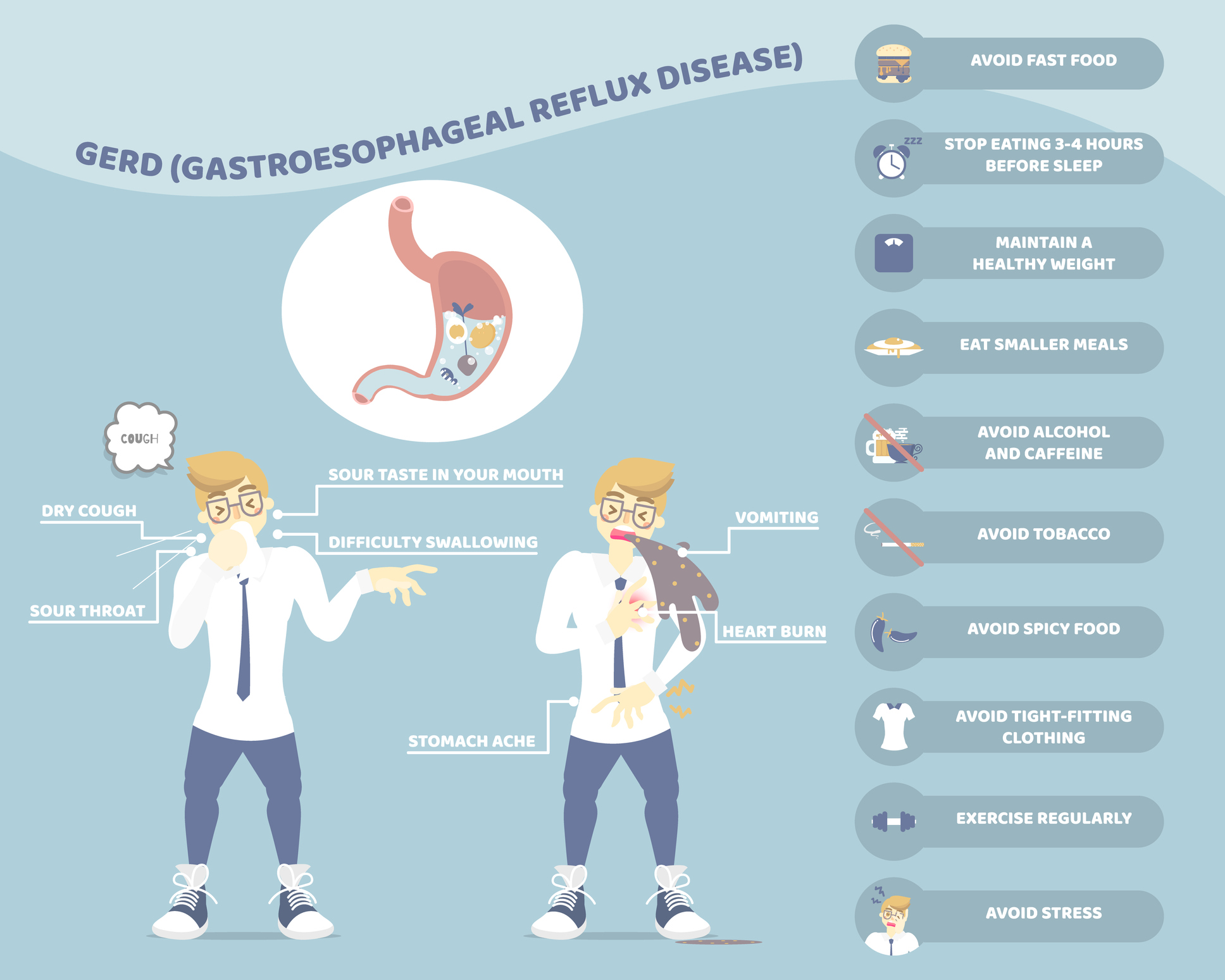
Symptoms of Acid Reflux Disease (GERD)
The symptoms for acid reflux and the symptoms of GERD are the same; they just happen more frequently with GERD.
Symptoms of acid reflux include:3
- Heartburn, a burning sensation or pain in the chest that can move up into the neck and throat. The pain can be so severe that it can be mistaken for heart attack.
- Regurgitation of food or sour liquid
- Nausea
- Chronic cough or hoarseness
- Difficulty swallowing or painful swallowing
Health Complications of GERD
The symptoms of GERD can lead to many health problems if untreated. Here are just a few of them.
Esophagitis
Esophagitis is inflammation of the lining of the esophagus. It is the most common complication of GERD, occurring in about 50% of patients.4
If untreated, esophagitis can damage tissues of the esophagus and lead to Barrett’s esophagus, increasing the risk of esophageal cancer.
Common symptoms of esophagitis include:5
- Heartburn
- Sore throat
- Regurgitation of acid
- Pain or difficulty swallowing
- Chest pain that occurs after eating
- Food becoming stuck in the esophagus
- Cough
- Decrease in appetite
In those too young to explain their discomfort, such as infants, symptoms may include feeding difficulties and/or insufficient weight gain known as “failure to thrive”.
Untreated esophagitis can lead to painful ulcers and scarring of the esophagus. It can even cause esophageal stricture, a severe narrowing of the esophagus that constitutes a medical emergency.
Barrett’s Esophagus
Barrett’s esophagus is characterized by an abnormal change in cells present in the lower part of the esophagus. Specifically, the flat pink cells lining the esophageal tissue are replaced with thick red ones resembling those lining the intestines.
Barrett’s esophagus may increase the risk of developing esophageal cancer, though this risk is small.
The exact cause of this condition is unknown, but esophageal damage from frequent acid reflux is believed to play a role. Barrett’s esophagus is mostly seen in those with long-term GERD. However, only 10% to 15% of those with GERD develop this condition.6
Symptoms of Barrett’s esophagus include:
- Difficulty swallowing food
- Frequent heartburn
- Regurgitation of acid and other stomach contents
- Vomiting blood
- Blood in the stool
- Weight loss
Many people, however, have no symptoms, especially in the early stages.
Esophageal Ulcers
An esophageal ulcer is a painful sore located in the lining of the lower part of the food pipe, where the esophagus meets the stomach.
It is a type of peptic ulcer that can be caused by acid reflux eroding the esophageal lining. However, this type of ulcer is most often caused by a Helicobacter pylori bacterial infection.
Symptoms of esophageal ulcers include:
- Burning pain in the chest
- Loss of appetite
- Nausea
- Vomiting
- Heartburn
- Indigestion
- Sour taste in the mouth
- Stomach pain
- Weight loss
- Internal bleeding
Esophageal Stricture (Narrowing of the Esophagus)
An esophageal stricture is characterized by a gradual narrowing of the esophagus. This makes swallowing difficult, as it prevents food and liquids from traveling to the stomach.
Though GERD is the most common cause of stricture, it can also be caused by cancer or by eosinophilic esophagitis, an allergic reaction that inflames the esophagus.
Symptoms of esophageal stricture include:
- Difficulty or discomfort swallowing foods and in some cases liquid, a condition called dysphagia
- The sensation of food stuck in your food pipe or chest area
- Weight loss
- Regurgitation of food
- Acid reflux symptoms, such as heartburn and stomach pain
Aspiration Pneumonitis
Aspiration pneumonitis occurs when a large amount of gastric contents are regurgitated and then inhaled (aspirated) into the lungs.
Gastric acid burns the airway and lungs. This can lead to lung inflammation, infection, or airway obstruction.
Symptoms of aspiration pneumonitis include:
- Chronic cough
- Chest discomfort/pain
- Fever
- Difficult or labored breathing (dyspnea)
Asthma
Though asthma and GERD may appear to be unconnected, there does indeed appear to be a link between the two. For instance, more than 75% of those with asthma also have GERD.7
Seems acid reflux can cause a “reflex arc” through the nervous system for the lung area, causing a reflex spasm of the bronchial tubes. This can lead to asthma or chronic cough.8
Symptoms of asthma include:
- Labored breathing
- Wheezing
- Coughing
- Shortness of breath
If you experience some or all of these systems and have GERD, your asthma may have been trigged by persistent acid reflux.
Neurological Inflammation
Neurological inflammation is not often discussed in relation to acid reflux or GERD, but research suggests that it does indeed play a role.
How does this work?
Well…let’s talk about systemic inflammation first. You see, chronic systemic inflammation is extremely common. It’s also damaging to health, as research indicates that inflammation may be the trigger for most chronic diseases.
Inflammation is your body’s response to tissue injury and is a crucial part of the immune system. As part of the healing process, your body releases pro-inflammatory mediators, such as cytokines. This triggers acute inflammation that gradually recedes as the injury heals. Acute inflammation lasts for just a few days to a couple of weeks.
Chronic inflammation occurs when the inflammatory response lingers for months or years. Over time, this can damage your tissues and organs. And it appears that the main culprit in both acute and chronic inflammation are pro-inflammatory cytokines.
Normally blood immune cells can’t cross the blood-brain barrier (BBB)9, which is why the brain has it’s own immune system governed by microglia cells. These cells stand guard to intercept any harmful substance that manages to breach the BBB.
Over time, systemic inflammation can damage the BBB10, allowing pro-inflammatory cytokines to enter the brain. This activated microglia cells that then call more pro-inflammatory cytokines to the scene for help, further damaging the BBB. This results in chronic brain inflammation.11
And due to a complex communication system between the gut and the brain (gut-brain axis)12, inflammation in the brain induces more inflammation in the body and vice versa. This positive feedback loop helps sustain chronic inflammation in the brain and the body.
But what does any of this have to do with acid reflux or gastroesophageal reflux disease?
Well…studies suggest that acid reflux triggers the esophagus to make cytokines, which leads to inflammation that damages the esophageal lining.13 In other words, it may not be chemical burns but inflammation that’s the real culprit in GERD.
GERD Risk Factors
There are several things that may increase your risk of GERD and/or aggravate the condition. Some factors thought to increase the risk of GERD include:
- Being overweight or obese, as excess weight puts pressure on the lower esophageal sphincter
- Pregnancy, for the same reason as above
- Smoking, as nicotine promotes excess stomach acid and relaxes the lower esophageal sphincter
- Hiatal hernia, a condition in which an opening in the diaphragm allows the upper stomach to move up into your chest
- Taking certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and Calcium channel blockers
- Connective tissue disorders, such as scleroderma
- Delayed stomach emptying
Factors that Aggravate GERD
Factors that can aggravate GERD and make the symptoms worse include:
- Smoking
- Eating certain foods
- Eating close to bedtime
- Eating too much food
- Using aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs)
- Eating heavily processed foods, especially sugar
Foods that Trigger Symptoms of GERD
Several different foods and beverages can trigger heartburn and other symptoms of GERD including:
- Fried foods
- Spicy foods
- Tomato
- Chocolate
- Pineapple
- Citrus fruit
- Garlic
- Fatty foods
- Mint
- Onion
- Garlic
- Soda
- Tea
- Coffee
- Alcohol
It’s important to note, however, that not everyone responds to the same foods in the same way. What food gives you heartburn may not affect someone else.
How is Acid Reflux and GERD Diagnosed?
To diagnose acid reflux and GERD, your doctor will give you a physical examination and ask you about your symptoms. They may be able to diagnose GERD based on symptoms alone.
To confirm the diagnosis, however, your doctor may recommend tests that include:
- Upper endoscopy, in which a long thin tube with a light and camera attached is inserted down your throat to examine the condition of your stomach and esophagus.
- X-ray of your stomach, esophagus, and upper intestine.
- Manometry, which measures movement and pressure inside the esophagus
Treatment Options for GERD
Here are just a few of the many treatment options for acid reflux and GERD.
Medications
Prescription medications and OTC remedies are great treatment options for acid reflux and the symptoms of GERD. These include:
- Antacids to neutralize stomach acid, e.g., Rolaids, Alka-Seltzer, Maalox, etc.
- Proton pump inhibitors to reduce production of acid in the stomach, e.g. Prilosec, Nexium, Prevacid (Some of these medications require a prescription.)
- Prokinetics to help strengthen the lower esophageal sphincter, thus helping to reduce or prevent acid reflux
- Foaming agents to prevent stomach contents from refluxing into the esophagus, e.g. Gaviscon
Surgery
If your acid reflux symptoms are severe and not soothed with medication or some of the diet and lifestyle changes listed below, your doctor may recommend surgery.
The main types of surgery — the LINX device and fundoplication — are minimally invasive and involved tightening and reinforcing the lower esophageal sphincter to prevent reflux.
If medication and diet/lifestyle changes don’t improve your symptoms of acid reflux, talk to your doctor about a surgical solution.
Diet and Lifestyle Changes
One of the best ways to treat acid reflux, though, is to implement some easy diet and lifestyle changes. Here a a few ways to treat acid reflux naturally.
Avoid trigger foods (See above for foods known to promote acid reflux)
- Eat smaller meals
- Stop Smoking
- Eat at least 3 hours before bedtime
- Elevate your head with a couple pillows when you go to bed
- Reduce or eliminate heavily processed foods from your diet. These foods typically loosen the lower esophageal sphincter and promote reflux.
- Lose weight (if overweight)
- Wear loose clothing and belts. (Tight clothing/belts put pressure on the stomach, causing acid to up towards the esophagus.)
- Get regular exercise, as this can improve digestion. Be sure to choose low-impact exercises that keep you upright, though, as bending over can trigger reflux.
SANE Vitaae Can Help
Say goodbye to painful heartburn, regurgitation, and other symptoms of acid reflux! This new brain-boosting nutraceutical is the first clinically proven formulation created to soothe neurological inflammation, the hidden cause of acid reflux. It contains all 4 of the brain-boosting super nutrients — folate, citicoline, CoQ10, and L-carnitine — in the correct combinations and dosages you need to heal any neurological inflammation that has occurred. Click here to learn more about Vitaae and to place your orders today while supplies last!
References
3- National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & Causes of GER & GERD. NIH. Last Reviewed Jul 2020. Accessed Apr 29, 2021. https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/symptoms-causes
4- Patti MG. How common is esophagitis as a complication of gastroesophageal reflux disease (GERD)? Medscape. Updated: Oct 16, 2020. Accessed Apr 29, 2021. https://www.medscape.com/answers/176595-45395/how-common-is-esophagitis-as-a-complication-of-gastroesophageal-reflux-disease-gerd#:~:text=Esophagitis%20(esophageal%20mucosal%20damage)%20is,is%20demonstrated%20on%20barium%20esophagram.
5- Mayo Clinic Staff. Esophagitis. Mayo Clinic. Feb. 23, 2021. Accessed Apr 29, 2021. https://www.mayoclinic.org/diseases-conditions/esophagitis/symptoms-causes/syc-20361224
6- Phillips WA, Lord RV, Nancarrow DJ, Watson DI, Whiteman DC. Barrett’s esophagus. Journal of Gastroenterology and Hepatology. 2011;26:639–648.
7- Cleveland Clinic. GERD (Chronic Acid Reflux). Last reviewed: Dec 6, 2019. Accessed Apr 29, 2021. https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburn-overview
8- Lawrence L. Consider GERD in patients with pulmonary diseases. ACP Internist. Mar 2014. Accessed Apr 29, 2021.
9- Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol. 2015;7(1):a020412. Published 2015 Jan 5. doi:10.1101/cshperspect.a020412
10- Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017 Feb;60:1-12. doi: 10.1016/j.bbi.2016.03.010. Epub 2016 Mar 16. PMID: 26995317.
11- Aktas O, Ullrich O, Infante-Duarte C, Nitsch R, Zipp F. Neuronal Damage in Brain Inflammation. Arch Neurol. 2007;64(2):185–189. doi:10.1001/archneur.64.2.185
12- Newsmax Health. Inflammation is Direct Cause of Acid Reflux Damage. Apr 30, 2021. Accessed Apr 30, 2021. https://www.newsmax.com/Health/Health-News/inflammation-cause-acid-reflux/2016/05/19/id/729687/
13- Osadchiy V, Martin CR, Mayer EA. The Gut-Brain Axis and the Microbiome: Mechanisms and Clinical Implications. Clin Gastroenterol Hepatol. 2019 Jan;17(2):322-332. doi: 10.1016/j.cgh.2018.10.002. Epub 2018 Oct 4. PMID: 30292888; PMCID: PMC6999848.