Why did I poop in my sleep?
CLICK HERE TO Experience clean, and consistent perfect daily poops with increased youthful energy!
Are you haunted by the question, “Why did I poop in my sleep?” Read on to learn why bowel movements sometimes happen while sleeping and what you can do about it.
Experiencing a bowel movement during sleep can be deeply troubling and affect your mental state. After all, pooping the bed is not considered “normal” for most adults, as we’re supposed to be able to control our bathroom habits. But don’t despair. Once you know the reasons why you’re pooping in your sleep, it’s easier to find solutions.
Why Am I Pooping Myself In My Sleep?
Bowel movements occurring in bed at night will likely be loose and watery stool. This is known as nocturnal diarrhea, and it can be caused by a brief illness or a more serious disorder. Because it often wakes you up at night, it can negatively affect the quality of your sleep.
Symptoms of Nocturnal Diarrhea
Symptoms of nocturnal diarrhea include: 1
- Loose, watery stools
- Abdominal pain
- Nausea
- Fever
- Urge to poop
These symptoms typically last just a few days. But if they last more than a couple weeks, it may be a sign of a more serious condition. See your doctor if they persist for more than a few days.
Dangers of Diarrhea
Whether it occurs during the day or at night, diarrhea can be dangerous to your health. This is because severe diarrhea can cause a depletion of water and electrolytes, leading to dehydration and serious health problems. Elderly people and young children are especially at risk for serious complications of dehydration.
According to research, around 20% to 30% of older adults are dehydrated.2 There are several reasons for this including an age-related decrease in body fluids. In most cases, the dehydration is minor. But if an older person develops diarrhea, it can quickly progress to severe dehydration if fluid isn’t replaced. This may require hospitalization.
Severe dehydration from diarrhea can be especially dangerous for elderly individuals, as their bodies are more susceptible to fluid imbalances. It’s also important to note that, for certain individuals, weight loss drugs may contribute to gastrointestinal symptoms, including diarrhea, particularly if they are not used under proper medical supervision. For individuals already at risk of dehydration, this could further complicate their health. If you are considering weight loss drugs, it’s essential to consult with a healthcare provider to ensure they are suitable for your situation and to minimize potential side effects.
Causes of Nocturnal Diarrhea
Here are a few conditions known to cause nocturnal diarrhea.
Infections
Viral, bacterial, and parasitic infections often create watery stools, a.k.a, diarrhea. Infections known to promote diarrhea include:3
- Viral: Norovirus, Rotavirus
- Bacterial: e Coli, Salmonella (These are foodborne infections, e.g., “food poisoning”.)
- Parasitic: Cryptosporidium enteritis, Entamoeba histolytica (Parasitic infections are most often transferred through infected drinking water, and are also food borne infections.)
In some cases, infections can affect both the stomach and the small/large intestines, causing inflammation of the gastrointestinal (GI) tract known as gastroenteritis. (Viral gastroenteritis is stomach flu and is not caused by influenza virus.)4 This can result in diarrhea, nausea/vomiting, abdominal pain, and sometimes fever.
Though gastroenteritis can clear up on its own, you should see your doctor if diarrhea lasts for more than 2 days. That’s because it may be caused by other more serious conditions. Also a severe case of bacterial gastroenteritis is a medical issue that can lead to dehydration, kidney failure, and other dangerous conditions. 5
Foods
A variety of foods may cause diarrhea, including:
Dairy products
If you experience diarrhea after consuming dairy products, you may lack the enzyme necessary to break down the sugars in dairy. (This is known as lactose intolerance.) Because the body can’t break down these sugars, it often disposes of it through loose and watery bowel movements. About 36 percent of people in the U.S. are thought to be lactose intolerant.6
Gluten-containing grain foods
Gluten is a protein found in wheat, barley, and rye grains. (This includes foods made with white flour, as it’s made from milled wheat grain.) Those with “gluten sensitivity” are unable to break down or digest gluten, resulting in diarrhea and other gut issues. Experts believe around 6 percent of the U.S. population may be gluten sensitive. That’s 20 million people! Plus, one in 133 people in the U.S. are believed to have Celiac disease, a serious condition in which gluten damages the intestines.7
High-fiber foods
Fiber is a natural substance found in grains, fruits, and vegetables. Though dietary fiber is necessary for regular bowel movements, too much fiber too soon can be hard on your gastrointestinal tract. This often leads to diarrhea, cramping in the gut area, and other unpleasant symptoms. To avoid diarrhea, increase your fiber intake slowly. This gives your digestive tract a chance to adjust to it.
For certain individuals using weight loss drugs, being mindful of these dietary triggers is particularly important, as some medications may interact with food sensitivities or amplify gastrointestinal discomfort. Adjusting your diet to reduce potential irritants can help minimize these side effects and support overall digestive health while using weight loss medications.
CLICK HERE TO Experience clean, and consistent perfect daily poops with increased youthful energy!
Coffee
There is no doubt that a cup of coffee in the morning can wake you up fast…but it can also promote diarrhea. That’s because the caffeine in coffee stimulates the bowels. To reduce your chances of diarrhea, try to limit yourself to just 1 cup of coffee per day. Two or more cups of coffee or caffeinated tea can lead to diarrhea. 8
Caffeine-containing foods
A common cause of diarrhea is consuming too many caffeine-containing foods, e.g., chocolate, tea, most sodas, etc. This has the same bowel-stimulating effect as drinking coffee.
Fruit
Though eating fruit is good for your health, it also contains a natural sugar called fructose that may cause loose stool and diarrhea. This is more likely to occur if you eat a large amount of fruit.9 To avoid runny stool, try to eat fruit in moderation. Also, choose low-fructose fruit as much as possible. Citrus fruits and berries are popular low sugar options.
Medications And Supplements
Certain medications are a common cause of watery stool. Medications that may lead to diarrhea include:10
- Laxatives: Laxatives are designed to make stool softer and easier to pass. However, taking too many laxatives could promote diarrhea.
- Magnesium: This mineral draws water into the intestines, thereby softening the stool. It can also relax the muscle of the intestines, helping make stool easier to pass.
- Antacids: Most antacid brands contain magnesium, which can lead to diarrhea.
- Antibiotics: As a treatment for infectious conditions, antibiotics work well. However, a common side effect of antibiotics is that they destroy certain types of bacteria. This can lead to an imbalance of good and bad gut bacteria that can result in diarrhea.
- Chemotherapy medications (a common treatment for cancer)
- NSAIDS (non-steroidal anti-inflammatory drugs) used to treat pain and arthritis, e.g., aspirin.
- Heartburn medications, e.g., Prilosec
Medical Conditions
Several different chronic medical conditions can cause nocturnal diarrhea. Here are a few health conditions known to trigger diarrhea during sleep, as well as sporadic diarrhea during the day.
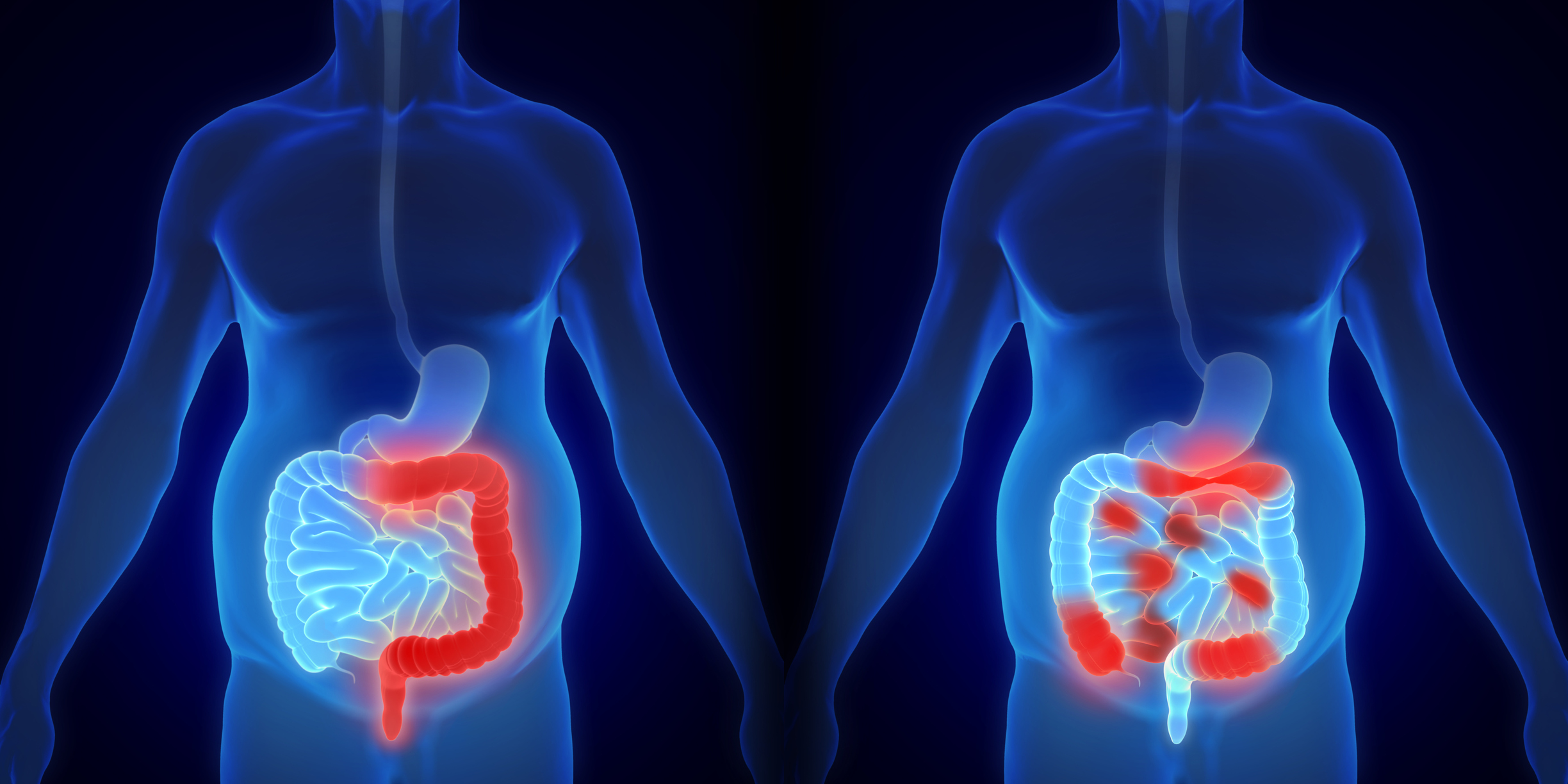
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease, or IBD, is chronic inflammation of the GI tract. The cause of inflammatory bowel disease is unknown, but researchers believe an autoimmune response — in which the immune system mistakenly attacks healthy cells — plays a role.
There are 3 types of IBD: ulcerative colitis, Crohn’s disease, and microscopic colitis.
- Ulcerative colitis promotes chronic inflammation of the inner lining of the large intestine (colon) and rectum, causing painful ulcers (sores) in your GI tract. Signs many include may include bloody diarrhea, pain in the rectum, and fever.11 However, the signs of of ulcerative colitis vary greatly depending upon the part of the digestive tract affected.
- Crohn’s disease is a chronic condition causing inflammation anywhere in your GI tract, including the rectum. Symptoms of Crohn’s can be mild or severe, and they can even go into remission for awhile. In addition to nocturnal diarrhea, signs of Crohn’s may include fatigue, stomach cramps, fever, and blood in the stool.12
- Microscopic Colitis is another chronic condition of inflammation of the colon. Your doctor can detect it only by examining your colon with a microscope. The symptoms are often sporadic and may include chronic diarrhea, nausea, and stomach pains/cramping.13
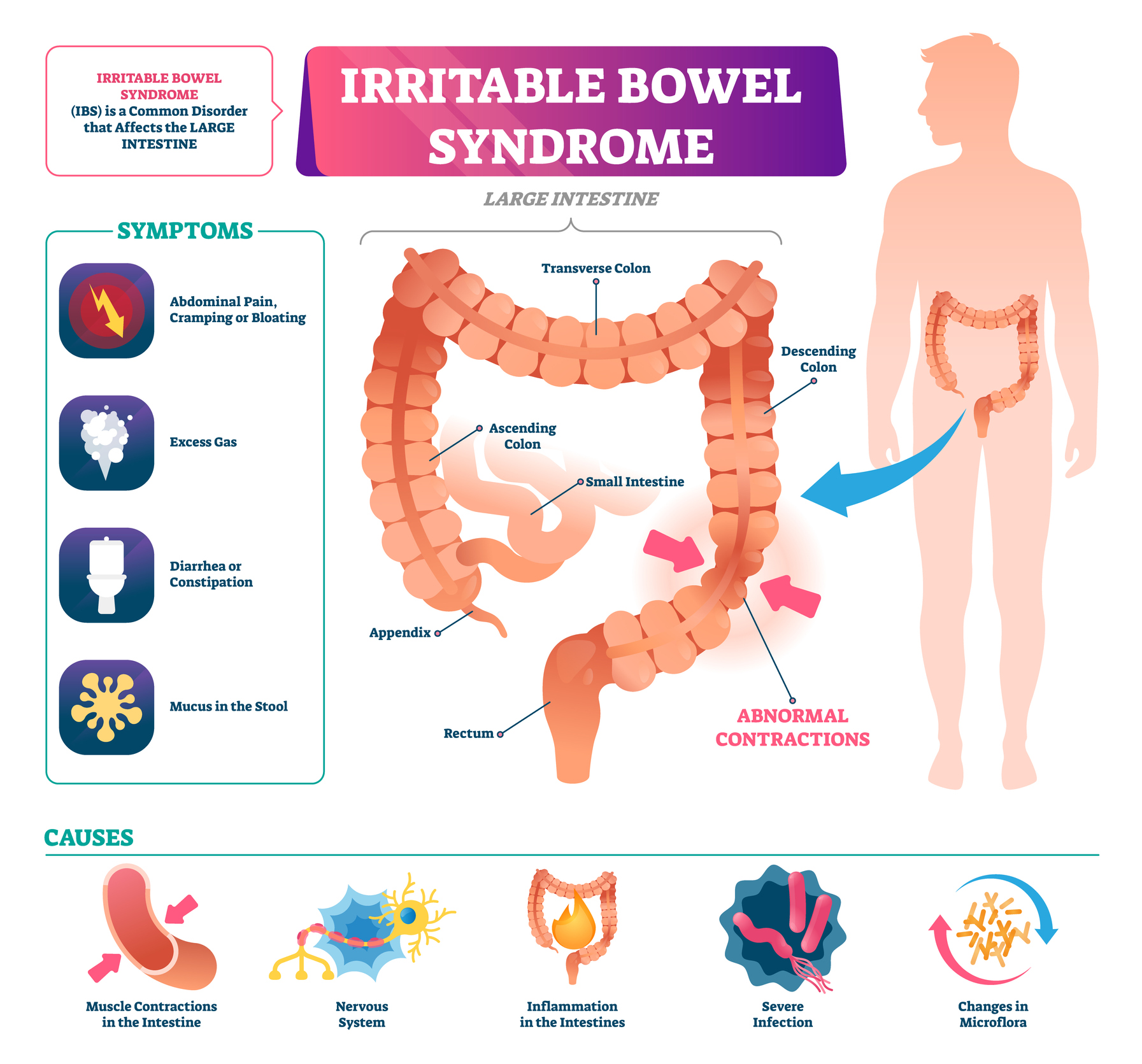
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a chronic condition that affects the large intestine. However, unlike inflammatory bowel disease, IBS does not appear to damage the GI tract. This is because IBS is a functional disease, that is, a disorder in which the gut and brain don’t work together properly.
Symptoms of IBS include abdominal pain/cramping, bloating, gas, pressure in the rectum, and diarrhea. However, nocturnal diarrhea is not a typical sign of IBS. For this reason, you should call your doctor if you experience diarrhea while you sleep. 14
Diabetes
Diabetes is a condition that affects the way the body uses glucose (blood sugar.) In type 1 diabetes, the pancreas doesn’t produce insulin and requires injections of insulin. In type 2 diabetes, the pancreas either doesn’t produce enough insulin or the cells don’t respond to insulin well.
With either type, glucose can build up in the bloodstream and cause medical complications. One of these complications is having diarrhea while you sleep.
Diarrhea is not that main sign of diabetes, however. Symptoms of diabetes vary and include increased thirst, irritability, and frequent urination. If you experience any of these signs, speak with your doctor.
Treatment for Pooping While Sleeping
It’s not fun pooping at night while you sleep. Not being able to control your bowels while sleeping can make you feel helpless and embarrassed.
The good news is that there is a treatment — several of them — that can help keep you from pooping while you sleep. The treatment you choose depends upon the reason for this issue, and any advice from your doctor.
Here are a few things you can do to avoid pooping during sleep:
- Take an anti-diarrheal medicine, such as Pepto-Bismol
- Avoid foods and beverages known to have a laxative effect, e.g., prune juice, coffee
- Eat only bananas, rice, applesauce, and toast until your symptoms ease. This is called the “BRAT” diet, and it’s commonly prescribed for diarrhea because these foods are easy to digest.
- Make dietary adjustments that eliminate “problem” foods. For instance, if you know you’re lactose intolerant, avoid dairy foods.
- Avoid any triggers that may cause a flareup of your IBD or IBS symptoms.
- Try to manage your blood glucose levels if you have diabetes
When To See A Doctor
Nocturnal diarrhea typically resolves within a couple of days without medical treatment. But if diarrhea continues for more than 2 days, call your doctor. As previously mentioned, diarrhea can be a symptoms of a more serious condition, and it can also cause dehydration.
Could You Use Some Help With Poop Control?
CLICK HERE TO Experience clean, and consistent perfect daily poops with increased youthful energy!
Pooping in your sleep happens sometimes. But it doesn’t need to control your life. Though fixing your poop issues could seem hopeless at times, it’s easier than you may think. You can improve regularity and enjoy complete satisfying poops with a patented molecule that is backed by Harvard doctors! Click here to learn more about this groundbreaking poop fix formula and to place your order TODAY.
References
1- Leonard J. What causes diarrhea in the middle of the night? MedicalNewsToday. May 26, 2018. Accessed Mar 12, 2021. https://www.medicalnewstoday.com/articles/321936
2- Miller HJ. Dehydration in the Older Adult. J Gerontol Nurs. 2015 Sep 1;41(9):8-13. doi: 10.3928/00989134-20150814-02. PMID: 26375144.
3- National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & Causes of Diarrhea. NIH. Nov 2016. Accessed Mar 12, 2021. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea/symptoms-causes
4- National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & Causes of Diarrhea. Symptoms & Causes of Viral Gastroenteritis (“Stomach Flu”). NIH. May 2018. Accessed Mar 15, 2021. https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/symptoms-causes
5- National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & Causes of Diarrhea. Symptoms & Causes of Viral Gastroenteritis (“Stomach Flu”). NIH. May 2018. Accessed Mar 15, 2021. https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/symptoms-causes
6- National Institute of Diabetes and Digestive and Kidney Diseases. Definition & Facts for Lactose Intolerance. NIH. Feb 2018. Accessed Mar 15, 2021.https://www.niddk.nih.gov/health-information/digestive-diseases/lactose-intolerance/definition-facts
7- Anderson J. How Many People Have Gluten Sensitivity? Medically reviewed by Priyanka Chugh, MD October 25, 2020. Very Well Health. Accessed Mar 15, 2021. https://www.verywellhealth.com/how-many-people-have-gluten-sensitivity-562965#:~:text=According%20to%20Dr.%20Fasano%2C%20gluten%20sensitivity%20potentially%20affects,the%20United%20States%20alone%20could%20have%20the%20condition.
8- International Foundation for Gastrointestinal Disorders. Last Updated: Oct 2, 2019. Accessed Mar 15, 2021. https://www.iffgd.org/lower-gi-disorders/diarrhea/common-causes.html
9- International Foundation for Gastrointestinal Disorders. Last Updated: Oct 2, 2019. Accessed Mar 15, 2021. https://www.iffgd.org/lower-gi-disorders/diarrhea/common-causes.html
10- Mammadli R. List of Medications that Cause Diarrhea. Health Recovery. Aug 31, 2016. Accessed Mar 15, 2021. https://iytmed.com/list-medications-cause-diarrhea/#:~:text=Descriptions%20of%20Medications%20that%20Cause%20Diarrhea%201%20They,also%20cause%20diarrhea%20or%20make%20it%20even%20worse.
11- Mayo Clinic Staff. Ulcerative Colitis. Mayo Clinic. Accessed Mar 15, 2021. https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
12- Mayo Clinic Staff. Crohn’s Disease. Mayo Clinic. Accessed Mar 15, 2021. https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
13- Mayo Clinic Staff. Microscopic colitis. Mayo Clinic. Accessed Mar 15, 2021. https://www.mayoclinic.org/diseases-conditions/microscopic-colitis/symptoms-causes/syc-20351478
14- Leonard J. What causes diarrhea in the middle of the night? MedicalNewsToday. May 26, 2018. Accessed Mar 15, 2021. https://www.medicalnewstoday.com/articles/321936
Types of poop one encounters is categorized by the Bristol Stool Chart. This chart is a generalized indicator of how or why different types of poops look and feel a certain way. The 7 types of poop are broken up into categories based on a 2,000-person study!
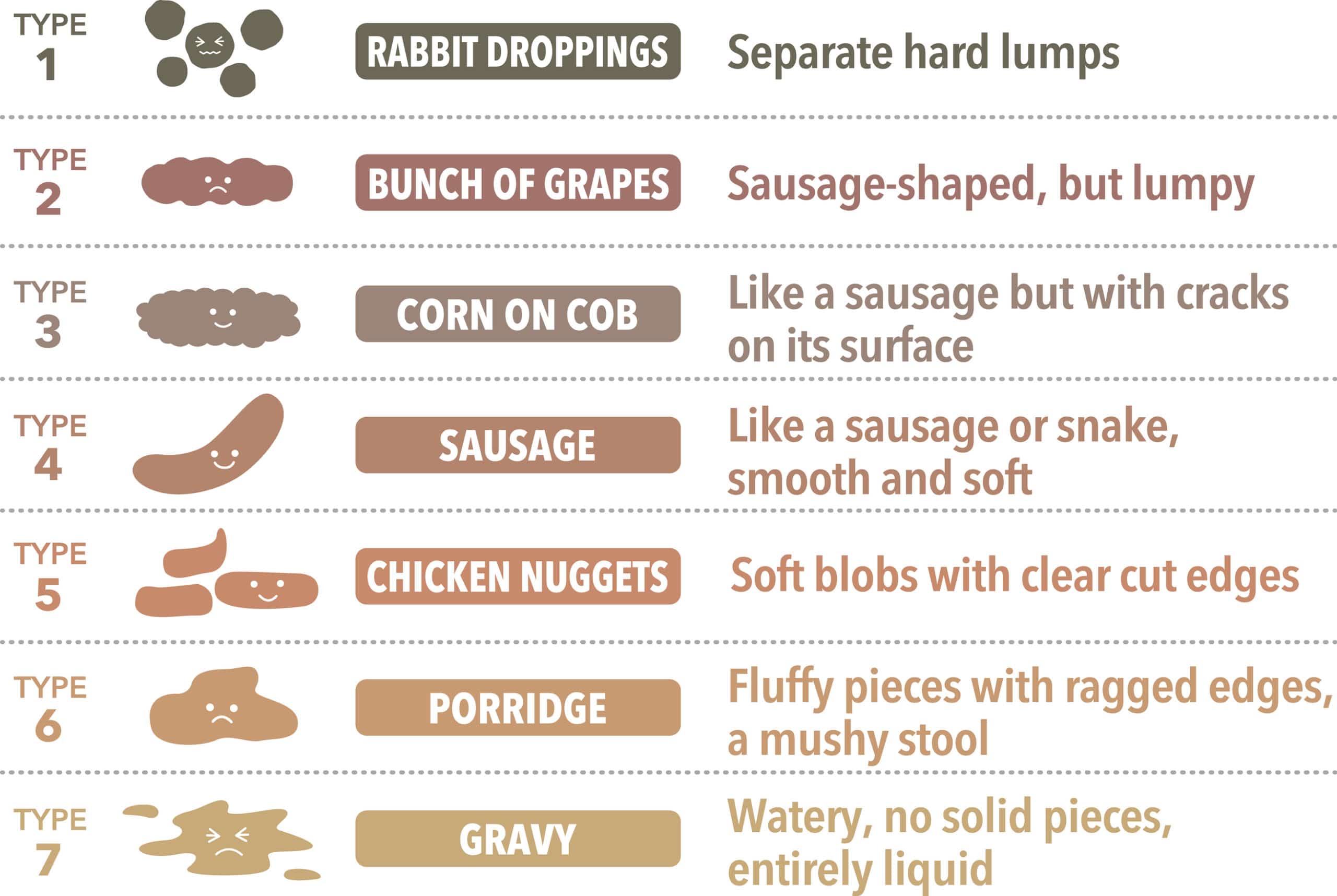
Does your poo look this good? If you have Bristol Type 3 or 4 – your poop is considered “normal”! Bristol Type 1 or 2, is where the poop is hard and difficult to pass, are indicative of constipation. Often, these types of stool can be painful to pass – but don’t worry – Doctor Poo has a recommended healthy-gut switch solution…just keep reading!
Should you ever worry about your poop?
Always consult your healthcare provider if you have any concerns about what your poop means. People are asked to call their health care providers if: They experience severe levels of abdominal pain or discomfort with diarrhea that does not go away when you poop or fart. Also, if diarrhea is accompanied by fever of 101 degrees Fahrenheit or higher, chills, vomiting, or fainting, call your physician immediately.
What is an unhealthy poop?
An unhealthy poop is when one poops too often (hence, your doctor asking you if you poop more than three times daily) or not pooping often enough (As such, less than three times a week) and also excessive straining when pooping. Poop that is colored red, black, green, yellow, or white. greasy, or fatty stools is unhealthy.
Help fix so many of your digestive and bathroom issues, such as gas and bloating and improve your overall health with this patented molecule that is backed by Harvard Doctor’s by clicking here!
Doctor Poo Provides More Valuable Answers for Those Hard to Ask Questions Below: